Table of Contents
ToggleProstate cancer remains one of the most common malignancies among men, often spreading beyond the prostate to other parts of the body. When it metastasizes to the bones, it can significantly impact a patient’s quality of life and lead to severe complications. Understanding the progression from prostate bone metastasis to death is crucial for patients, families, and healthcare providers alike.
This journey often involves complex interactions between cancer cells and the bone microenvironment, resulting in debilitating pain and other symptoms. As survival rates improve, the focus shifts from merely extending life to enhancing the quality of life during treatment. By exploring the mechanisms behind prostate bone metastasis and its implications, one can gain valuable insights into better management strategies and support for those affected.
Overview of Prostate Bone Metastasis
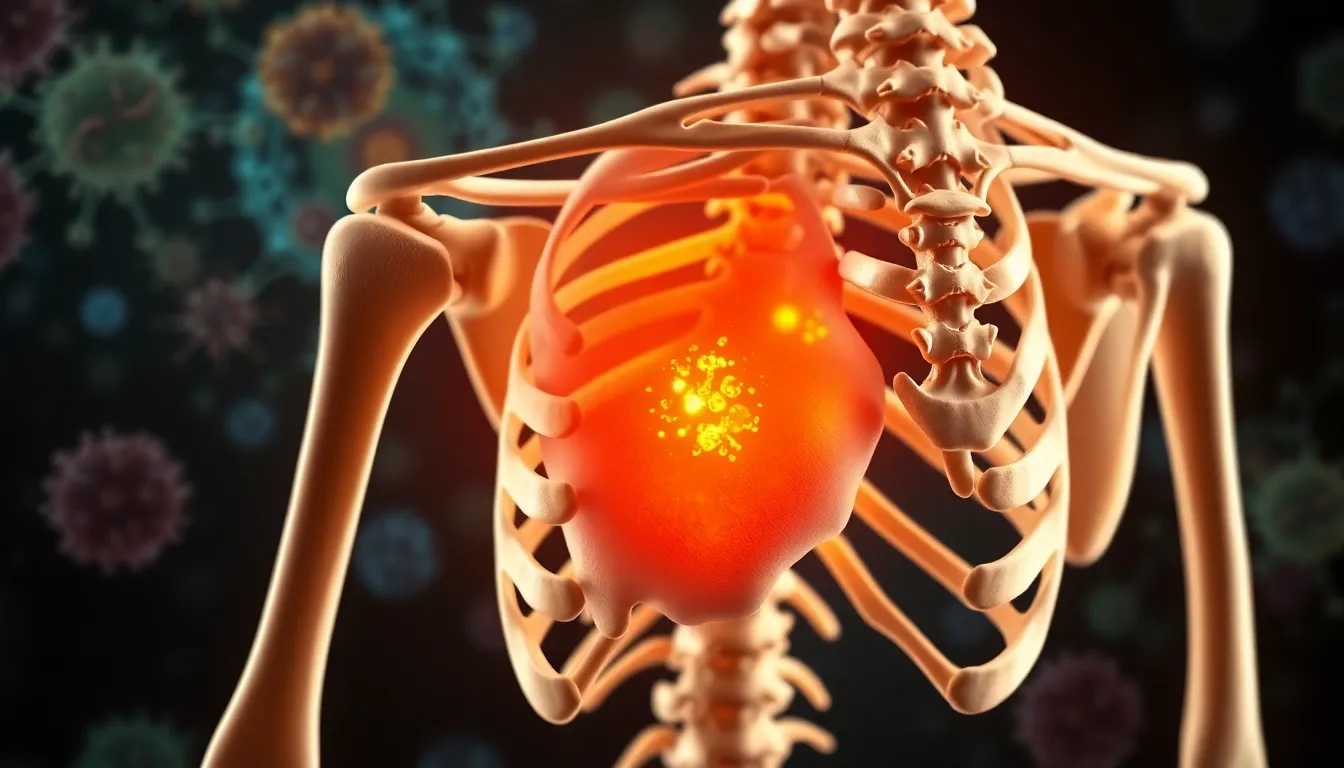
Prostate cancer commonly metastasizes to bones, occurring in approximately 70% of advanced cases. The metastasis process involves prostate cancer cells spreading to bone tissue, which disrupts normal bone metabolism. This disruption leads to bone pain, fractures, and other complications that significantly impair patient quality of life.
Cancer cells interact with the bone microenvironment through numerous signaling pathways. These interactions promote tumor growth and can trigger osteoblastic or osteolytic lesions. Osteoblastic lesions involve excessive bone formation, while osteolytic lesions cause bone resorption and weakening.
Pain management becomes critical due to the debilitating symptoms associated with bone metastasis. Bisphosphonates and denosumab are commonly prescribed to reduce complications like skeletal-related events, including fractures and spinal cord compression.
As survival rates for prostate cancer improve, patients often face prolonged periods with metastasis. This extension of life necessitates a shift in focus towards managing symptoms and maintaining quality of life during treatment. Understanding the biological mechanisms behind prostate bone metastasis aids healthcare providers in developing more effective support strategies for those affected.
Mechanisms of Prostate Bone Metastasis
Prostate bone metastasis involves intricate biological processes that facilitate the spread of cancer cells to the bone. Understanding these mechanisms offers insights into potential therapeutic targets.
Cellular Pathways Involved
Cellular pathways play a crucial role in the metastatic process. Prostate cancer cells utilize several signaling pathways to promote their survival and growth in bone tissue.
- PI3K/Akt Pathway: This pathway contributes to increased cell survival and proliferation, allowing metastatic cells to thrive in the bone environment.
- MAPK/ERK Pathway: This pathway facilitates cellular migration and invasion, enhancing the ability of cancer cells to penetrate bone tissues.
- Wnt/β-catenin Signaling: This signaling network influences osteoblast and osteoclast activity, creating a favorable environment for tumor growth in the bone.
- Intracellular Communication: Cancer cells communicate with bone cells through cytokines, such as IL-6 and TNF-α, promoting both osteoblastic and osteolytic activity depending on the metastatic context.
Role of the Microenvironment
The bone microenvironment significantly impacts prostate cancer metastasis.
- Bone Matrix Composition: The unique composition of the bone matrix provides a nurturing environment for prostate cancer cells, facilitating their adhesion and colonization.
- Osteoclast Activation: Tumor cells secrete factors that stimulate osteoclast activation, leading to increased bone resorption and release of growth factors, which further promote tumor growth.
- Immune Cell Interaction: Immune cells in the bone marrow can either suppress or support tumor progression, influenced by factors such as regulatory T cells and myeloid-derived suppressor cells.
- Hypoxia: The bone environment may exhibit low oxygen levels, which can drive cancer cells to adapt through activation of hypoxia-inducible factors, promoting angiogenesis and further metastasis.
Understanding these mechanisms aids in developing more effective therapeutic strategies targeting prostate bone metastasis, ultimately impacting patient outcomes.
Diagnosis of Prostate Bone Metastasis
Accurate diagnosis of prostate bone metastasis requires advanced techniques and reliable biomarkers. These methods help in detecting the presence of metastatic lesions and assessing their impact on patients’ health.
Imaging Techniques
Imaging plays a crucial role in diagnosing prostate bone metastasis. Common techniques include:
- Bone Scintigraphy: This scan detects areas of increased bone metabolism indicative of metastatic lesions. It shows the entire skeleton, allowing for the identification of both osteoblastic and osteolytic changes.
- Magnetic Resonance Imaging (MRI): MRI provides detailed images of bone and surrounding soft tissues, helping detect lesions in early stages. It defines the extent of the disease.
- Computed Tomography (CT): CT scans offer cross-sectional images of bones and other tissues, aiding in pinpointing metastatic sites, especially in combination with other imaging techniques.
These imaging methods enhance diagnostic accuracy and guide treatment planning.
Biomarkers for Detection
Biomarkers assist in the diagnosis and monitoring of prostate bone metastasis. Key biomarkers include:
- Prostate-Specific Antigen (PSA): Elevated PSA levels often indicate disease progression. While not specific to bone metastasis, it provides insight into overall cancer activity.
- Alkaline Phosphatase (ALP): High ALP levels can suggest increased bone turnover due to metastatic activity. Monitoring ALP helps assess treatment response.
- Bone Turnover Markers: Markers such as N-telopeptide and C-telopeptide reflect bone resorption and can indicate the presence of metastases.
Utilizing these biomarkers, healthcare providers gain valuable information for diagnosing and managing prostate bone metastasis effectively.
Treatment Options for Prostate Bone Metastasis
Various treatment options exist for managing prostate bone metastasis. These options aim to control disease progression, alleviate symptoms, and improve patients’ quality of life.
Systemic Therapies
Systemic therapies target metastatic prostate cancer cells throughout the body. These include:
- Hormonal therapy: This involves androgen deprivation therapy (ADT) to lower testosterone levels, which can slow down the growth of prostate cancer cells. Common agents include GnRH agonists like leuprolide and anti-androgens such as enzalutamide.
- Chemotherapy: Docetaxel and cabazitaxel are commonly used chemotherapeutic agents, meant to attack cancer cells directly and improve survival rates in advanced stages.
- Radium-223: This alpha-emitting radioactive isotope specifically targets bone metastases, providing significant pain relief and improves overall survival in symptomatic patients with bone metastases.
- Targeted therapies: Recent advancements include PARP inhibitors, such as olaparib, which are effective in patients with mutations in DNA repair genes like BRCA1/2.
Palliative Care Strategies
Palliative care strategies focus on improving quality of life and managing symptoms. These strategies include:
- Pain management: Opioids and non-opioid analgesics, along with therapies like radiation, effectively relieve bone pain associated with metastasis.
- Bisphosphonates and Denosumab: These medications reduce skeletal-related events (SREs), including fractures and spinal cord compression. They help strengthen bones and reduce pain levels by inhibiting osteoclasts, which are responsible for bone resorption.
- Physical therapy: Customized exercise programs can enhance mobility and strength, helping patients manage symptoms and maintain functionality.
- Psychosocial support: Addressing emotional and psychological challenges through counseling or support groups is vital for enhancing patients’ overall well-being.
Focused treatment plans involving these systemic therapies and palliative care strategies can lead to improved management of prostate bone metastasis, alleviating symptoms and enhancing patients’ quality of life.
Prognosis and Survival Rates
Prognosis for patients with prostate bone metastasis varies significantly based on several factors, including disease stage, treatment response, and overall health. The median survival rate for men with metastatic prostate cancer is approximately 3 to 5 years. However, survival rates significantly decline for patients presenting with extensive metastasis or those with specific complications, such as epidural spinal compression.
Survival rates also depend on the extent of skeletal involvement. Research shows that patients with isolated bone metastases often fare better than those with visceral organ involvement, such as the liver or lungs. Average 5-year survival rates for men with bone-only metastasis range from 30% to 51%, while those with additional organ metastasis experience substantially lower rates.
Advancements in treatment options have also impacted prognosis. The introduction of androgen receptor-targeted therapies, radium-223, and other systemic treatments have demonstrated improved survival outcomes. Clinical trials indicate that new agents can extend survival by months, sometimes reaching 2 to 3 additional years in specific patient populations.
Pain management and palliative care play a vital role in enhancing survival quality. Patients receiving comprehensive pain management strategies often report a better quality of life, which can indirectly influence survival. Research underscores the necessity of individualized care plans that incorporate systemic treatments alongside supportive measures to ensure optimal patient outcomes.
Regular monitoring of markers such as Prostate-Specific Antigen (PSA) and Alkaline Phosphatase (ALP) allows healthcare providers to track disease progression effectively. Early intervention and modifying treatment plans based on these markers can lead to better management of prostate bone metastasis.
Prostate bone metastasis presents significant challenges for patients and healthcare providers alike. Understanding its complexities is essential for improving patient outcomes and quality of life. As research advances and treatment options evolve, a multifaceted approach that combines effective pain management with targeted therapies can lead to better management of symptoms and disease progression.
With a focus on personalized care and regular monitoring, patients can navigate the difficulties of prostate bone metastasis more effectively. By prioritizing both physical and emotional well-being, the healthcare community can enhance the overall experience for those affected by this condition.